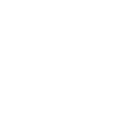
Interstitial Lung Disease (ILD)
It covers a huge spectrum of disorders with complex interplay of clinical symptoms and diagnostic challenges.
It is a group of disorders which makes the lungs shrink progressively with passage of time. Effective and early diagnosis can slow down the progression in most cases of these complex spectrum of disorders and reverse the damage in a selected few.
Our department has pioneered the concept of DPLD clinic with advanced bronchoscopy, lung function testing and rehabilitation services.
We also have twice weekly Multi-Disciplinary Team (MDT) discussion of all DPLD/ILD cases with thoracic radiologists.
Our team consists of consultants with special interest in various ILDs who have received advanced training in India and overseas.
We also have close liaison with Rheumatology and Immunology department within our Vellore town campus , which shares a lot of overlap of our cases.
The usual treatments involve patient centric rehabilitation, immunosuppressive agents, antifibrotics and vaccinations. These are decided after careful evaluation and detailed discussion among the experienced consultants of our department and other concerned departments.
The Common Conditions Referred or Treated:
- IPF – Idiopathic Pulmonary Fibrosis – IPF
- HP- Hypersensitivity Pneumonitis – CHP
- NSIP – Non-specific Interstitial Pneumonia
- Sarcoidosis
- Vasculitis affecting lungs
- Interstitial Lung Diseases related to connective tissue diseases
- Drug induced lung diseases
- Occupational lung diseases
- OP – Organizing Pneumonia
- RBILD – Respiratory Bronchiolitis Interstitial Lung Disease
- DIP – Desquamative Interstitial Pneumonia
- AIP – Acute Interstitial Pneumonia
- LIP – Lymphocytic Interstitial Pneumonia
- PPFE – Pleuro-parenchymal fibroelastosis
- CPFE – Combined pulmonary fibrosis and emphysema
- LAM – Lymphangioleiomyomatosis
- LCH – Langerhans Cell Histiocytosis
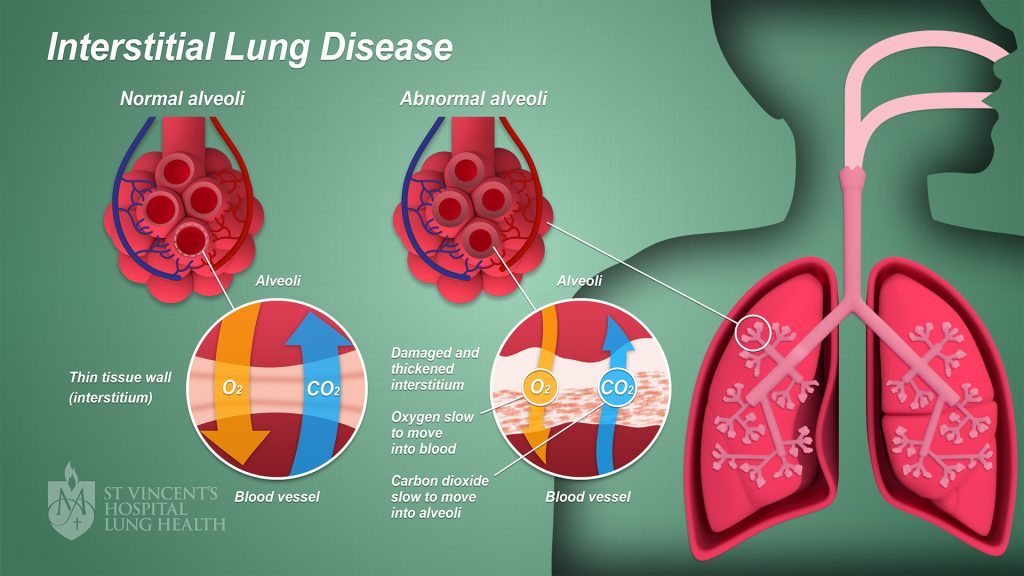
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a disorder that is characterized by obstructive apneas, hypopneas and/or respiratory effort related arousals caused by repetitive collapse of the upper airway during sleep. It is the most common sleep related breathing disorder. Factors that contribute to the etiology of OSA are:
- Obesity
- Short neck
- Small mandible/Receding mandible
- Male gender
It is important to diagnose and treat OSA because if left untreated, it can worsen Hypertension, arrhythmias and increase the incidence of vascular events like stroke and Myocardial infarction, impotence and decreased libido, cognitive impairments and driving accidents.
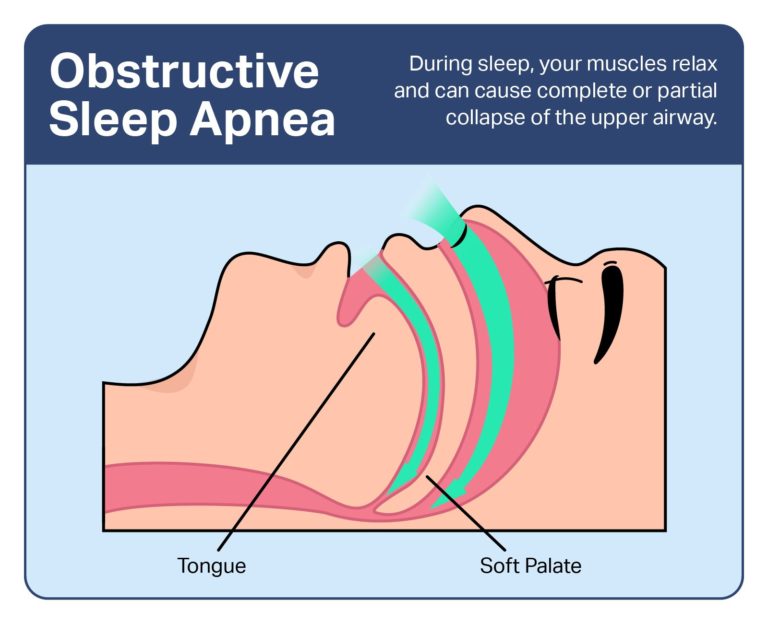
Pleural Diseases
Pleura is the serous membrane that covers the lung parenchyma, mediastinum, diaphragm and the rib cage. It is divided into parietal pleura and visceral pleura. Any injury, inflammation or infection cause blood or air or fluid to build up in this pleural space and causes pleural diseases. It can be pleurisy, pleural effusion, pneumothorax, hydropneumothorax etc.
Pleural Disorders:
- Pleural effusion: Caused by Infections, Primary and secondary tumors of pleura, Collagen vascular disorder etc. Can also be due to other systemic diseases like cardiac failure, renal failure or liver failure etc.
- Pneumothorax: It is the condition were air gets accumulated in pleural spaces
- Hemothorax: Presence of significant amount of blood in pleural space
- Primary or secondary Malignancy
- Ultrasound guided Diagnostic Thoracentesis
- Ultrasound guided Closed Pleural biopsy
- Ultrasound guided mass biopsy
- Medical Thoracoscopy
- Therapeutic Thoracentesis
- All modes of Intercostal drainage like Intercostal drainage tubes, Seldinger, Rockets, Indwelling pleural catheter etc.
Pulmonary Vascular Disorders
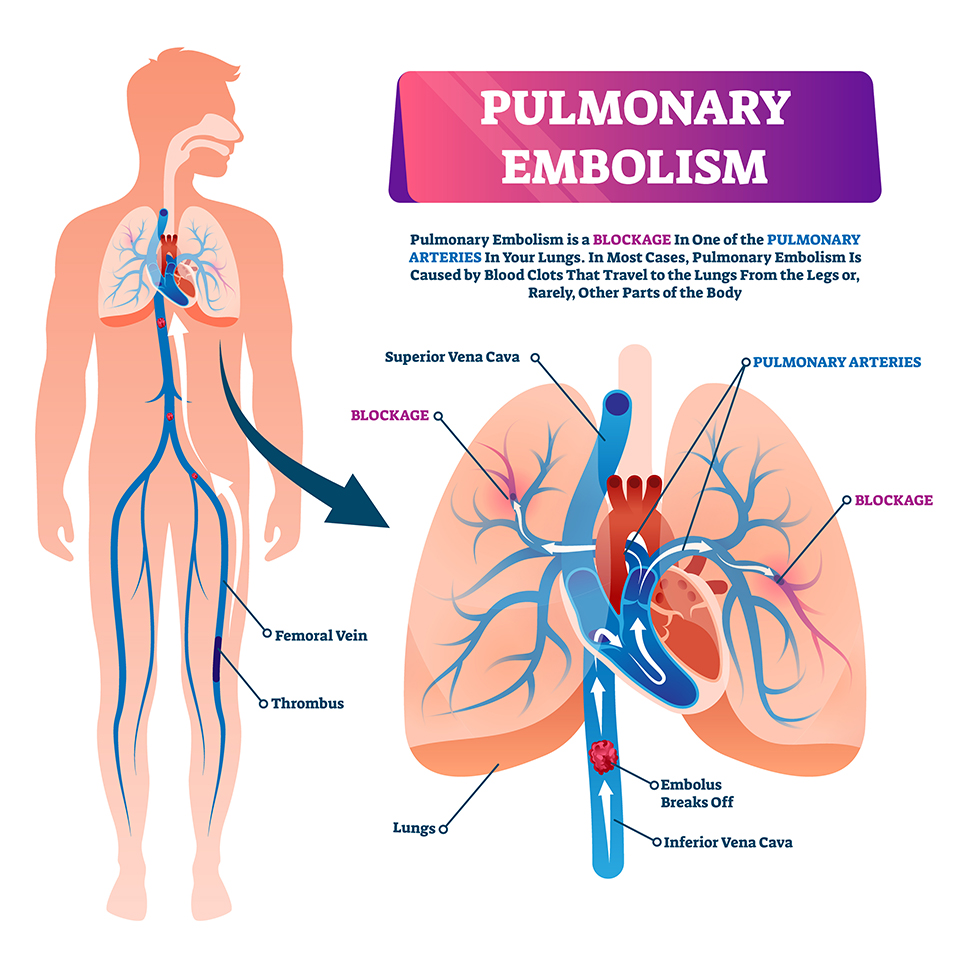
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death. Immediate treatment is very important.
Pulmonary hypertension (PH or PHTN) is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise, and in later stages, even to walk. If unidentified and left untreated, it can lead to right heart failure and death.
Asthma Allergy and Immunological Diseases
Conditions we treat
- Asthma
- Hives (Urticaria)
- Angioedema
- Food allergies
- Drug allergies
- Anaphylaxis
- Allergic Bronchopulmonary Aspergillosis
- Eosinophilia and Eosinophilic- related diseases
- Immune Deficiency and Immune Dysregulation Disorders
- Mastocytosis
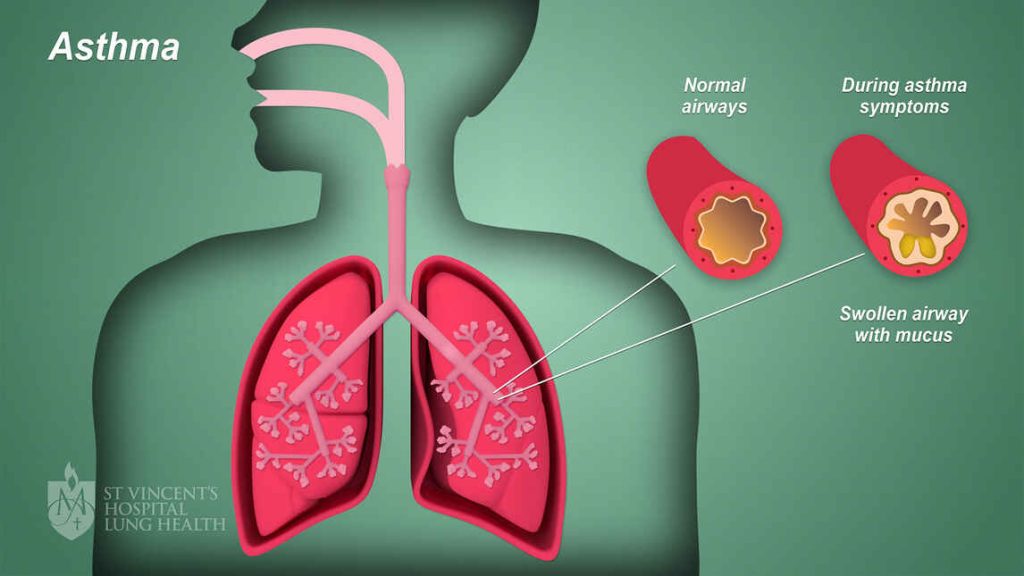
Asthma
- Asthma doesn’t have to hold you back and you don’t have to face it alone.
- We offer a personalised approach to your asthma- we understand your asthma is unique to you!
- Accurately diagnose asthma with acceptable clinical and diagnostic tests
- Identifying your asthma type and triggers which worsens your asthma
- We offer convenient, quality allergy shots/ drops (Immunotherapy)
- We offer biological treatment (Injections) if your symptoms are severe and not controlled with inhalers
- Spend time in educating you about your disease
- Education on environmental changes that would benefit your outcome
Why See a Specialist for Your Asthma?
- Asthma is common inflammatory disorder of the airways. It can affect some people only when they catch a cold or exercise while other people may have daily symptoms and have to alter their lifestyle because of asthma. Despite attempts to categorize patients, most experts agree that each individual's asthma acts differently and has different triggers. Furthermore, it can be silent and some asthmatics may have low grade symptoms and not feel it because they are able to compensate. This can be picked up on exam and with special tests performed by your doctor.
- Asthma can be life altering disorder that should be followed closely by a trained physician. There are many therapies that can accommodate all patients' treatment preferences and goals. By working closely with a trained specialist an asthmatic and their family will understand the choices available to them.
- Although no cure exists for asthma, excellent treatment is available for control of symptoms. We learn more about it every year, and newer, more effective and safer drugs are always being developed. As a result, most patients live normal, productive lives.
Allergies
Think again!
Hives (Urticaria) – Patient education info –provided below Angioedema
Food allergies – Patient education info – provided below
Drug allergies – Patient education info – provided below
Anaphylaxis – Patient education info – provided below
Hives (Urticaria)
When to Suspect Urticaria?
Urticaria is another term for “hives.” The condition affects an estimated 20 percent of the population at one time or another in their lives. An episode of hives can start as itching, followed by swollen, red welts. The itching may be mild or severe. Scratching, alcohol beverages, exercise and emotional stress may worsen the itching.
An episode of hives may last from a few minutes to several hours to several days to several weeks. Each individual welt should last no more than 24 hours.
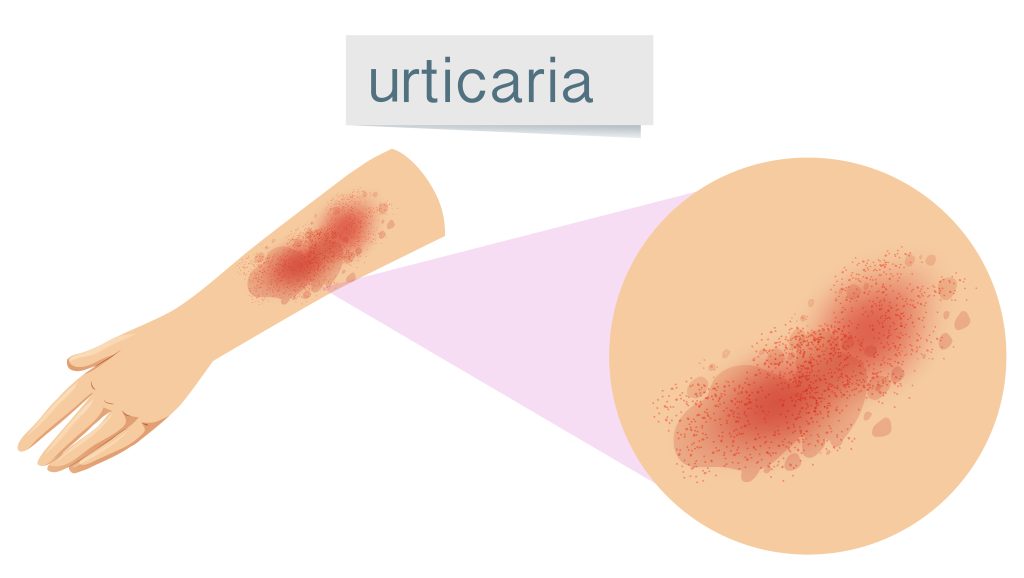
How Do I Get it Evaluated and Treated?
The specialist will take a detailed history about your medical history, your family’s medical history, your work and home environment, and medication you’re taking.
Allergy skin testing may provide useful information in some cases. Rarely, if food allergies are suspected, skin testing, elimination diet, and/or oral food challenges may be required. When vasculitis is suspected, a skin biopsy may be helpful.
The specific cause of urticaria can be identified in approximately 20 percent of cases.
In most instances, urticaria will improve with medications such as antihistamines. Severe episodes of urticaria may require temporary treatment with prednisone or a similar steroid medication.
We also provide biologics (Omalizumab) which is FDA approved for the treatment of Chronic Idiopathic Urticaria in patients who have symptoms despite antihistamines.
Food Allergies
Food Allergy in India
Traditionally, India has had a low incidence of food allergies, but this is slowly changing now, as lifestyles change and people become more prone to conditions like lactose intolerance and allergies to dust mites.
Amongst the food allergens, cocoa, cashew nut, coconut, sea food, peanut (groundnut), legumes and soya bean are the other common positive food allergens.
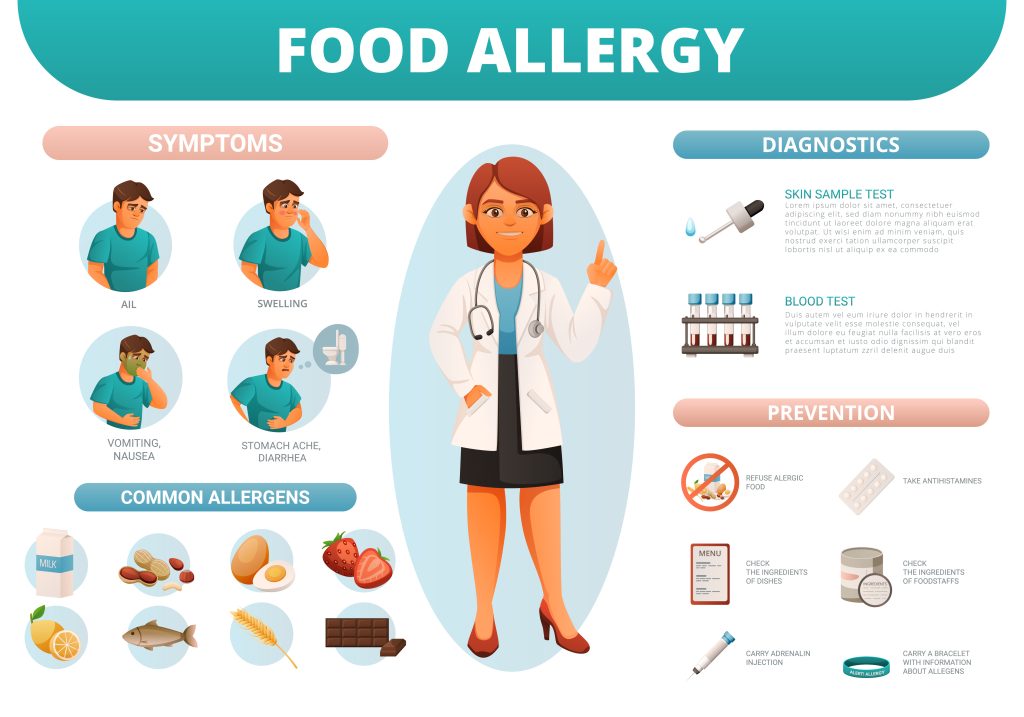
When Should I Suspect Food Allergy
Allergic reactions to foods typically begin within minutes to a few hours after eating the offending food.
The frequency and severity of symptoms vary widely from one person to another. Mildly allergic persons may only suffer a runny nose with sneezing, while highly allergic persons may experience severe and life-threatening reactions, such as asthma or swelling of the tongue, lips or throat.
The most common symptoms of food allergy involve the skin and intestines. Skin rashes include hives and eczema. Intestinal symptoms typically include vomiting, nausea, stomach cramps, indigestion and diarrhea. Other symptoms can be asthma, with cough or wheezing; rhinitis, often including itchy, stuffy, runny nose and sneezing; and rarely, anaphylaxis, a severe allergic reaction that may be life threatening.
What are My Options, if I Suspect Food Allergy
In our department, we offer one to one comprehensive consultation to understand your previous history of allergies with the offending food based on which we will plan further skin testing and oral challenge with your informed consent.
Drug Allergy
When Should I Suspect Drug Allergy
Drug allergy testing to common antibiotics, painkillers and anesthetic medications is offered in our department. Most people have probably experienced an unwanted side effect to a medicine at some time in their lives.
Allergic reactions can occur within minutes or hours of exposure to a medication. Drug reactions can even occur sometime after a medication has been stopped. For example, a person may develop a rash or hives a week after stopping a medication.
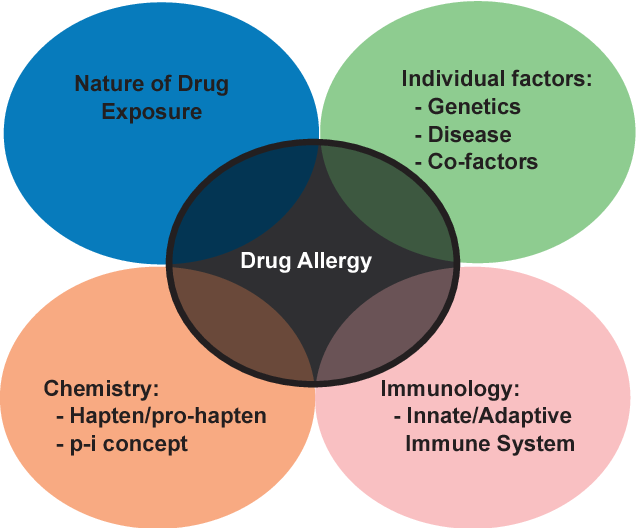
- Skin rash or hives
- Itchy skin
- Wheezing or other breathing problems
- Swelling of body parts
- Anaphylaxis, a life-threatening allergic reaction
What Should I do Next?
- Make sure your doctor knows the medication you took and the reaction you had
- Talk to your allergist about other medications you should avoid and which alternative medications are safe for you to take
- Plan your further testing and safe medications
What Are My Treatment Options?
- In our department, we offer one to one comprehensive consultation to understand your previous history of allergies with the offending drug based on which we will plan further skin testing and oral challenge with your informed consent.
- The main focus of drug allergy testing is to find safe alternative for you.
Anaphylaxis
What is Anaphylaxis?
Most people go through life without ever experiencing anaphylaxis — a rare but severe allergic reaction that occurs suddenly and can be life threatening. Anaphylaxis can happen moments, or even seconds, after being exposed to a triggering substance. For example, you may experience anaphylaxis directly following an insect sting or a penicillin shot. Because an anaphylactic episode can progress quickly, it is important to know the warning signs and prepare for an emergency episode if you have had an episode in the past.
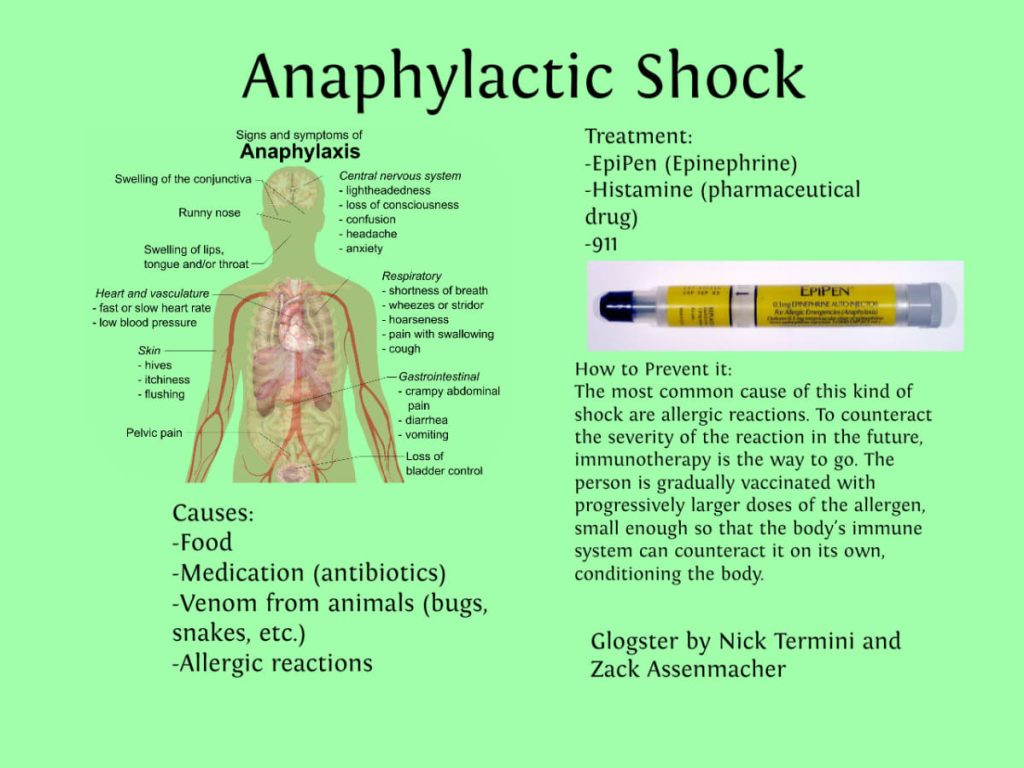
When To Suspect An Anaphylaxis?
- The symptoms and course of anaphylaxis can vary.
- Initial signs of an anaphylactic episode can be deceptively mild, such as a runny nose, a skin rash all over the body, or a nondescript “strange feeling.” These symptoms can quickly become more serious, including difficulty breathing, swelling of the throat or other parts of the body, rapid drop in blood pressure, and dizziness or unconsciousness.
Other symptoms of anaphylaxis include:
- Sense of impending doom
- Hives
- Tightness of the throat
- Hoarse voice
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Lightheadedness
- Cardiac effects, including a rapid drop in blood pressure and irregular heart beat
What Can Cause an Anaphylaxis?
The most common triggers include medications, food, insect strings and bites. Sometimes the trigger is not known.
It is important to seek immediate emergency medical care if you or someone you know begins to go into anaphylactic shock.
Things You Should Know/ Do, If You Had a Suspected Anaphylaxis
- Know your triggers. Avoiding the substances to which you are allergic is the most effective way to prevent future anaphylactic episodes.
- Know what to do if you unexpectedly come into contact with your trigger. Your doctor can help you develop a detailed plan of emergency care.
- Educate family and friends on what to do if you begin to have an anaphylactic episode.
- If your doctor has prescribed a self-injectable shot of epinephrine, carry it with you at all times.
- Keep a diary and being very aware of events that occur before episodes may ultimately help you find a trigger.
How Can We Help You?
Accurate diagnosis and successful management of allergies leading to anaphylaxis is essential. We help you diagnose the problem and help you develop a plan to protect you in the future.
Allergy Lab
We can test and treat allergies in children and adults. Options for food and drug allergies include skin testing (prick test, intradermal testing) followed by oral challenge if needed. Once testing is performed, we can help you determine the best course of treatment.
Our primary method for testing food and drug allergies is with a skin test. Allergy skin tests involve lightly pricking the skin with a tiny drop of the liquid food allergen. This is not painful. Some patients even say it tickles! An oral food challenge may be recommended if results from a skin test is uncertain. During this process, you’ll eat or drink small portions of the drug or food in increasing amounts over a period of time to see if an allergic reaction occurs. This is always done under a doctor’s supervision (in patient- setting).
Services We Provide in Our Allergy Lab:
- Environmental allergy skin testing
- Food allergy skin testing and oral challenge (In- patient setting)
- Drug allergy skin testing (prick testing, intradermal testing) and oral challenge (in-patient setting)
- Allergy shots/ injections
- Biologicals for Asthma and Hives patient
- Patient education and teaching for environmental allergen avoidance, food allergen avoidance, asthma education and epinephrine self- injection
Tuberculosis and NTM
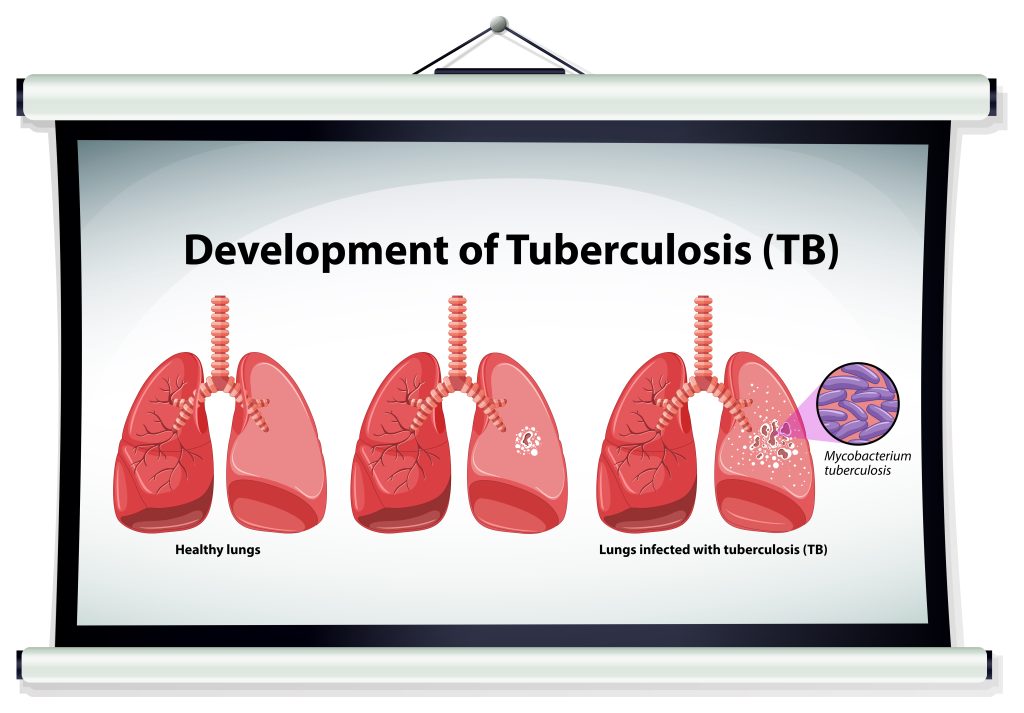
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body.
Typical symptoms of active pulmonary TB are chronic cough which is sometimes, blood stained, prolonged fever, night sweats, and loss of weight and appetite. It can also present with breathing difficulty and fluid collection within the covering of the lungs. Identification and proper treatment of this disease is very important.
Non Tuberculous Mycobacteria (NTM) also causes infection in the lungs, skin, lymph node etc. It commonly presents as chronic fever, cough with purulent expectoration, sometimes blood stained. It can mimic tuberculosis (TB) and hence, detailed evaluation is required for proper treatment.
Respiratory Medicine Dept
CMC Vellore
Christian Medical College
Ida Scudder Road,
Vellore – 632004
Tamil Nadu, India
Contact Info
Dept office number: 0416 2282859
Email: resmed@cmcvellore.ac.in
Working hours:
Mon – Fri: 8 am to 4.30 pm
Sat: 8 am to 12.30 pm
OPD Timing:
Wed: 8.00 am – 4.30 pm
Fri: 8.00 am – 4.30 pm
Sat: 8.00 am – 12.30 pm
Copyright © 2023 Dept. of Respiratory, CMC Vellore. All rights reserved. | Made with ❤️ by Akkenna.